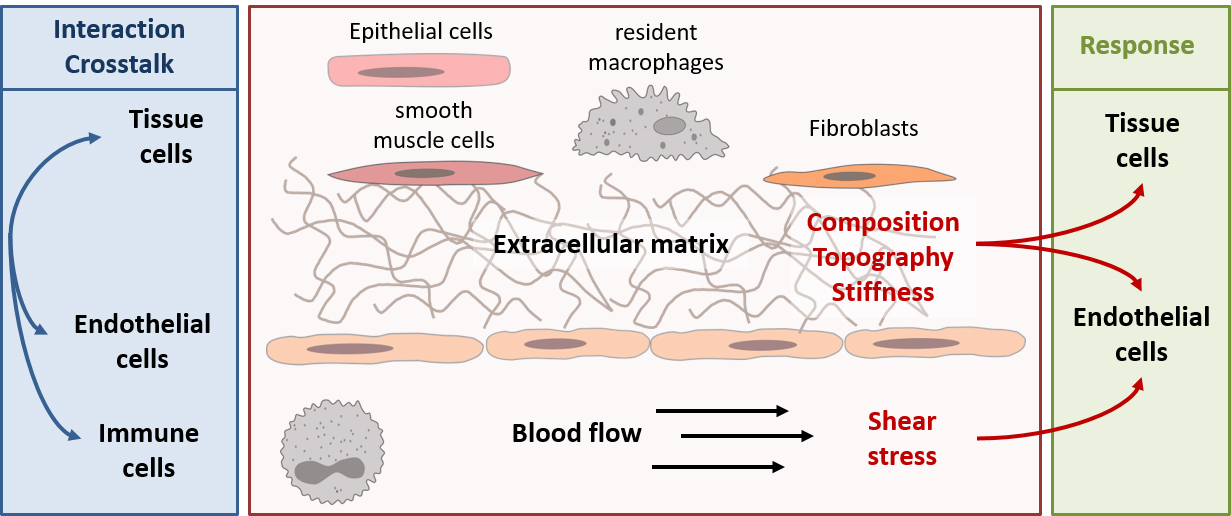
In the body, cells are permanently exposed to various mechanical forces. The endothelial cells lining the blood vessels are exposed to the frictional force of the blood flow (shear stress). Furthermore, in vivo cells are in permanent contact with their environment in which they grow. Depending on the region of the body, this environment differs in the composition and density of the cell types growing there and in the structure of the extracellular matrix. This leads to different mechanical properties, such as topography or stiffness, in this environment. Depending on the mechanical forces sensed by the cells, their phenotype, i.e. their expression pattern, the activity of different signaling pathways and, ultimately, their function changes. Therefore, it is not surprising that classical in vitro cell culture does not make it possible to reflect a physiological phenotype of cells. To change this, it is necessary to understand the influence of different mechanical forces on different cell types. This is exactly where we want to start. Our focus is on the investigation of mechanical forces that play a central role in blood vessels and their influence on inflammatory processes. It is our goal to create the basis to develop physiologically relevant in vitro models for vascular inflammation research, to reduce animal experiments according to the 3R principle (Replacement, Reduction and Refinement) and to provide important basic research for the development of new medical devices such as endothelialized implants.
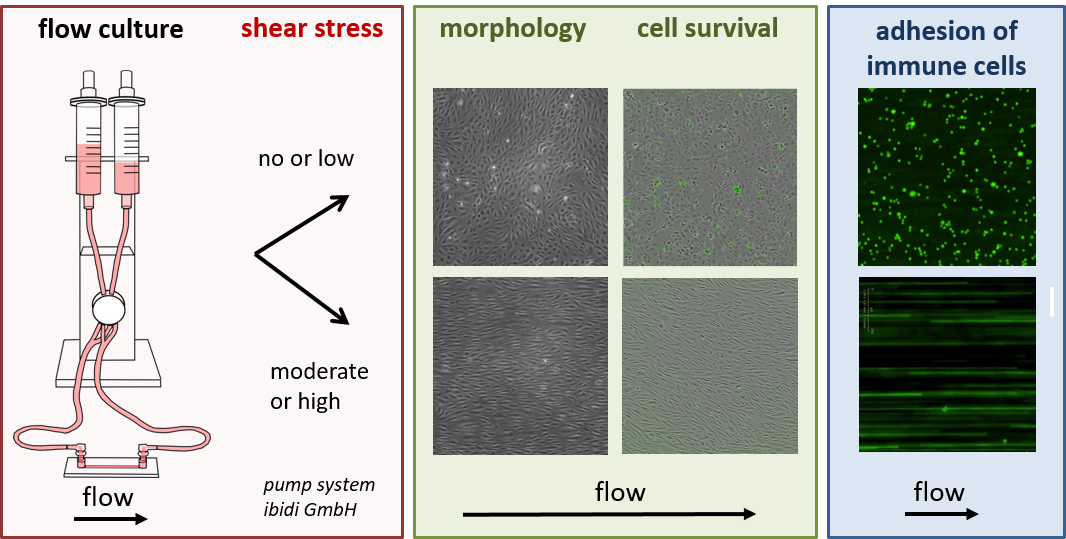
In first studies we investigated the protective and anti-inflammatory effect of flow culture on primary endothelial cells. In the course of our investigations we were able to show that proteases from the ADAM family are regulated by flow culture and contribute to the protective effect by increasing the survivability of the cells. Furthermore, we could show that pro-inflammatory factors, such as the membrane-bound chemokine CX3CL1, are strongly downregulated. In the case of CX3CL1, not only basal expression but also expression induced by the pro-inflammatory cytokine TNF was strongly inhibited by flow culture. This contributed to the fact that TNF-induced adhesion of monocytes to the endothelium was almost completely prevented during physiological flow culture.
In addition to flow culture, we are increasingly interested in the influence of substrate composition (composition, topography and stiffness) on various vascular cell types (such as endothelial cells and smooth muscle cells). In the future, we intend to extend our investigations to co-cultures in order to develop more complex cell culture systems under consideration of different mechanical forces and thus to create an in vitro system that is as physiological as possible. To achieve this we focus on interdisciplinary cooperations, which are closely linked in the Graduate School ME3T (www.me3t.rwth-aachen.de).
Career
We are always looking for motivated students for Bachelor's and Master's theses as well as for medical doctoral theses. If you are interested, please contact Dr. Aaron Babendreyer (ababendreyerukaachende).
Publications
- Differential Regulation of Lung Endothelial Permeability in Vitro and in Situ.
Uhlig, S., Yang, Y., Waade, J., Wittenberg, C., Babendreyer, A. and Kuebler, W. M. (2014). Cell. Physiol. Biochem. 34:1-19. - Shear Stress Counteracts Endothelial CX3CL1 Induction and Monocyte Cell Adhesion.
Babendreyer, A., Molls, L., Dreymueller, D., Uhlig, S. and Ludwig, A. (2017). Mediators Inflamm. 2017:1515389. - The metalloproteinase ADAM15 is upregulated by shear stress and promotes survival of endothelial cells.
Babendreyer, A., Molls, L., Simons, I., Dreymueller, D., Jahr, H., Denecke, B., Boon, R. A., Bette, S., Schnakenberg, U. and Ludwig, A. (2018). Submitted manuscript.


![[Translate to en:] [Translate to en:]](/fileadmin/files/global/_processed_/a/e/csm_Homepage_Header_Mosaik_Digitale_Patientenakademie_a70850c5a6.jpg)
![[Translate to en:] [Translate to en:]](/fileadmin/files/klinik-neurochirurgie/_processed_/f/a/csm__DSC8610_810ca6c404.jpg)


![[Translate to en:] [Translate to en:]](/fileadmin/files/klinik-neurochirurgie/_processed_/c/6/csm__DSC6827_8235404da8.jpg)


![[Translate to en:] [Translate to en:]](/fileadmin/files/global/_processed_/6/9/csm_Homepage_Header_Zahnprofis_neu_11014e086b.jpg)



![[Translate to en:] [Translate to en:]](/fileadmin/files/global/_processed_/5/d/csm_Homepage_Header_Pflege-Podcast_Schichtwechsel_ohne_Schriftzug_unten_9cef107de3.jpg)
![[Translate to en:] [Translate to en:]](/fileadmin/files/klinik-gynaekologie-geburtshilfe/_processed_/b/f/csm_Header_DSC1044_2762f31c37.jpg)
![[Translate to en:] [Translate to en:]](/fileadmin/files/klinik-urologie/_processed_/d/1/csm__ME27551_9b86eb20f4.jpg)
![[Translate to en:] [Translate to en:]](/fileadmin/files/global/_processed_/7/4/csm_Homepage_Header_Podcasts_2023_668979f13b.jpg)